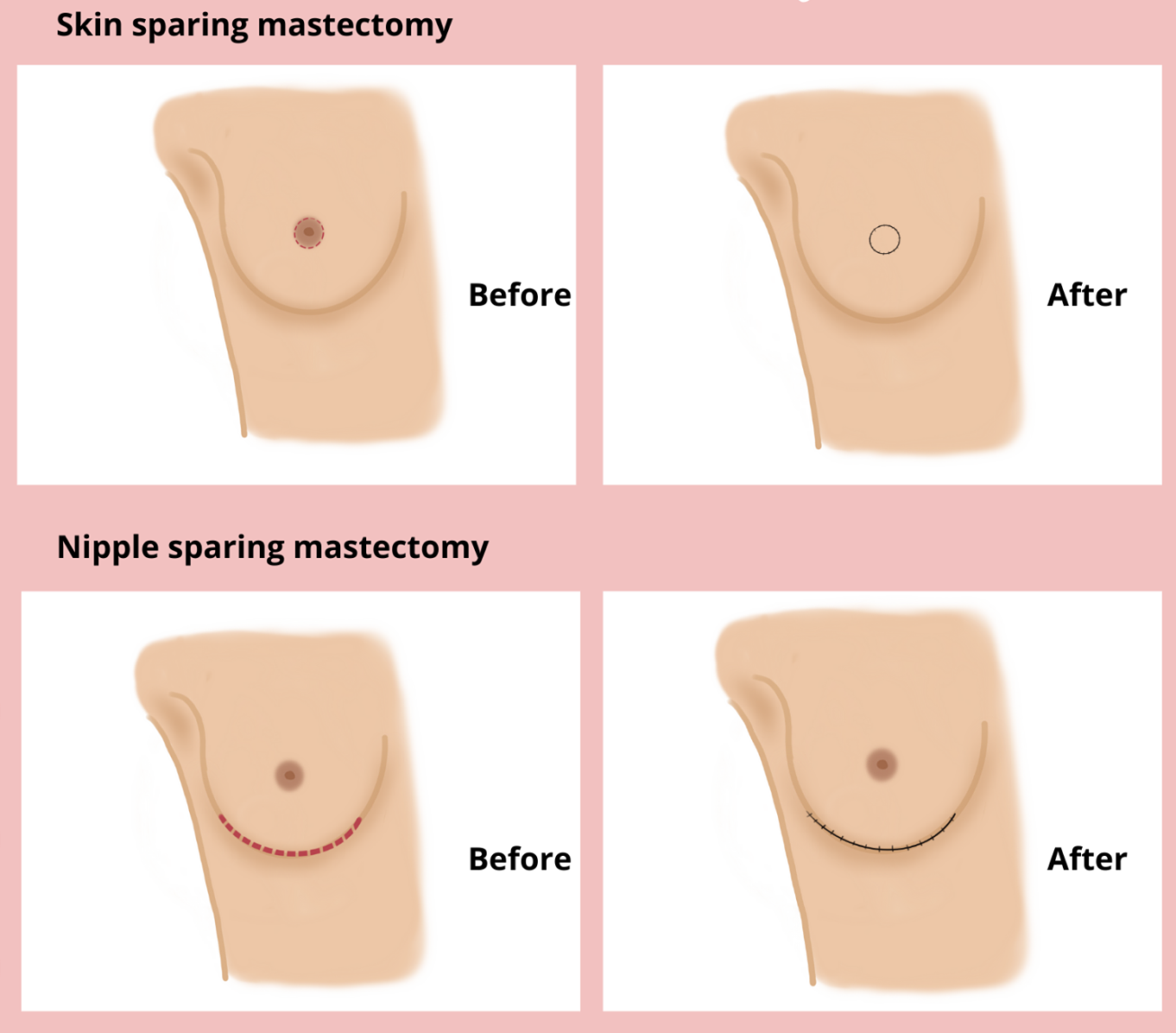
If your breast cancer does not affect much of the skin or need a risk-reducing mastectomy for genetic mutations like BRCA1/2 or PALB2, there is a possibility of preserving the skin envelope with a skin sparing mastectomy (SSM), or even, the nipple with a nipple sparing mastectomy (NSM), while removing the entire breast parenchyma. Both of these techniques are increasingly popular to treat early breast cancers when mastectomy is chosen. Both of these techniques are often coupled with breast reconstructive surgery with a plastic surgeon.
Both techniques have equivalent survival, when compared to a traditional mastectomy or lumpectomy.
Most patients are candidates for skin-sparing mastectomy except for those with inflammatory breast cancer or skin involvement.
The criteria for nipple-sparing mastectomy include: tumor size <3cm, tumor distance from nipple more than 2cm, clinically negative lymph nodes, no skin involvement or inflammatory cancer/Paget’s disease and preoperative breast MRI demonstrating no nipple involvement.
Oftentimes after NSM, the remaining skin and nipple are insensate, meaning there is minimal to no sensation. If sensation is desired, nerve preservation may be performed at the time of mastectomy in conjunction with the plastic surgeon.
If the decision is made to resect the nipple, patients may choose to have either nipple construction with the plastic surgeon or 3-D nipple tattoos.
Patients who have breast cancer and/or genetic mutations, such as BRCA1/2 are candidates for NSM or SSM.
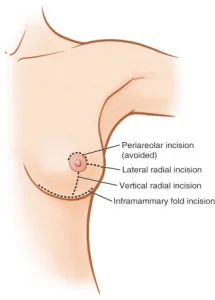
Incision for Nipple-Sparing Mastectomy